The intricacies of medical billing are a challenging task particularly, eligibility verification in medical billing. Today eligibility verification in fact is the most important part of medical billing; one step closer to faster reimbursement and a successful medical billing operation.
Eligibility Verification involves getting information from patients factually accurately and ensuring the information about the provider’s insurance, coverage by way of co-pays, deductibles, co-insurance and if pre-authorization is required for certain procedures; which can sometimes be very daunting and confusing.
Do you know – According to RemitData, two of the top five reasons for claim denials are directly tied to insurance coverage issues. Common causes include expired patient eligibility, where the insurance coverage is no longer valid on the date of service, and non-covered services, where the procedure is not included under the patient’s plan.
Despite over a decade of emphasis on improving eligibility verification processes, many practices still face significant challenges in this area. Improper or insufficient verification leads to millions of rejected claims each year, resulting in delayed payments and increased administrative costs. Establishing a robust insurance verification process can help prevent these denials, ensuring accurate claim submissions, reducing administrative burdens, and improving overall financial performance.
In fact, thus it’s crucial to verify insurance coverage before any clinical services are provided, rather than leaving this task to the billing team. Following a structured process for eligibility verification can significantly reduce the likelihood of eligibility-related denials. The Medical Group Management Association (MGMA) reports that healthcare providers see 5-10% of their claims denied. By reducing these denials through robust eligibility checks, practices can improve revenue and ensure greater financial stability.
What is Eligibility and Benefits Verification and its importance?
In its study, AMA established that eligibility or registration was considered a reason for 23.9% denied claims. Proper verification of eligibility greatly minimizes the percentages of claim denials that are caused by eligibility, among other errors, not only increases the revenue cycle but also accelerates cash flow. Proper eligibility verification is of great importance in preventing otherwise avoidable financial losses that accrue to the healthcare provider and streamlines the overall billing process.
With better pre billing services, ensuring accurate insurance verification in healthcare helps providers to have accurate and up-to-date information about a patient’s insurance coverage before delivering the particular services. In fact, it also helps in:
- Help Avoid Billing Errors – Avoid costly mistakes and billing errors due to incorrect or outdated insurance information when you provide healthcare services.
- Ensure Sound Income Sources – It will minimize claim denials to ensure that reliable income flows into your health care organization
- Increase Operational Cost Effectiveness – Administrative tasks and workload will be eased off to allow appropriate allocation of resources since your verification of insurance details happens proactively.
- Establish Trust and Transparency – This doctor-patient relation is likely to be trusted by a patient when transparent about their insurance information; therefore, no surprise or quarrel.
- Save Your Precious Time and Resources – This can be saved from your precious time by determination of insurance information beforehand. Therefore, all follow-up, administrative overheads, and other inefficiencies are avoided.
- Focused Patient Care – Do not interrupt the patient’s care. All the probabilities of interruptions in patient care shall get eradicated with clear information of their insurance, thus creating a streamlined and patient-centered health experience.
Information insurance companies needs:
- Subscriber name
- Patient name
- Patient’s relationship with the subscriber
- Patient’s date of birth
- Patient gender
- Patient member number
- Group name and number
- Plan type
- Coverage date (policy effective date)
Insurance verification elements
- Deductibles
- Co-pays
- Co-insurances
- Payable benefits
- Patient policy status
- Effective date
- Type of plan and all the coverage details
- Plan exclusions
- Claims mailing address
- Referrals & pre-authorizations
- Lifetime maximum, and more
ISSUES ON ACCOUNT OF THE LACK OF STRONG ELIGIBILITY AND BENEFITS VERIFICATION PROCESSES:
- Reduction in clean claims ratio
- Claim denials and consequently rework
- Delays in payment from healthcare payers
- Reduction in the profitability of the practice
Understanding the basics of the eligibility verification process
The steps involved in the eligibility verification process take place as follows:
Patient Scheduling:
Scheduling of patients via EDI, email or fax or check them every day in the appointment scheduling software.
2. Patient Enrolment:
Patient information is crucial for a seamless billing process so key data like the patient’s name, date of birth, address, diagnosis, allergies, and medical history. Additional details, such as emergency contacts, family doctors, and insurance providers, are typically recorded under specific categories.
3. Eligibility Verification:
Eligibility verification is key to the RCM process, improving clean claims and preventing payment issues. Regularly checking insurance coverage and updating patient information helps avoid errors. Informing patients about co-pays and deductibles ensures a smoother process.
4. Pre authorization:
Prior authorization is crucial in RCM, as payers must confirm approval for medications or procedures. Healthcare providers must wait for approval or contact insurance companies to complete the necessary steps if certain treatments or equipment are not approved.
5. Connecting Patients:
Patient data, including basic info, health records, and contact details, should be collected and maintained accurately. For additional information, like medication details, it’s best to contact patients directly for accuracy.
6. Billing System Update:
Medical billing software stores patient details, including insurance coverage. By using advanced verification systems to check insurance and verify eligibility with each visit, claim denials can be avoided.
How Sun Knowledge Ensures Best Practices for Accurate Eligibility Verification
Sun Knowledge experts improve your workflow with these strategies for accurate patient eligibility verification;
- By leveraging technology and automation: Sun Knowledge offers eligibility verification through automated systems eliminating the possibility of human error. These tools seamlessly interface with EHRs and practice management systems to run real-time coverage checks against payers’ databases.
- Collect complete patient information: By collecting full name, date of birth, provider of insurance coverage, policy number, and relationship to the policyholder, the expert allows for exact eligibility verification.
- Verify eligibility with every visit: Patients’ eligibility can be impacted by new work or changes in insurance. Prior to each visit, our expert verifying eligibility benefits the patient and the practice by preventing surprises at the end of the billing cycle.
- Record Financial obligations: Our expert discusses patients’ financial obligations when the patient first contacts your office, including deductibles and co-pays. Transparency increases patient satisfaction and discourages billing disputes.
- Establish a verification process: Ensure a systematic process for pre-visit, day-of-visit, and post-visit verification checks to ensure all coverage is verified with minimal opportunity for errors.
- Staff Training Cycle: Train your staff on the latest verification processes and payer requirements. Education helps keep efficiency and reduces errors in eligibility checks over time.
- Engage with Payers: Educate the insurance payers and form meaningful partnerships. This coordination ensures timely updates on coverage criteria and policy changes so that you can communicate best with people and verify efficiently.
- Denial Management: Even with best practices notwithstanding, every bit of organizational effort can result in some denials. A denial management system like ours can assist in analyzing trends, streamline processes, and eliminate eligibility-related denials’ root causes.
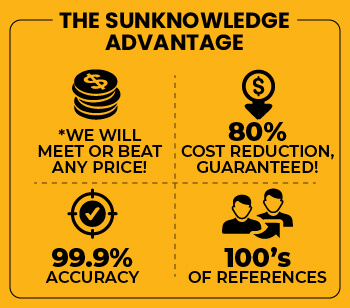
Simplify Your Insurance Process with Sun Knowledge’s Eligibility and Benefits Verification Services!
Are you facing challenges with eligibility and benefits verification? Our comprehensive services eliminate the uncertainty from insurance coverage, ensuring that your patients receive the necessary coverage while minimizing claim rejections and delays. We offer a flexible approach, receiving workflows through various patient scheduling systems such as EDI, Fax, emails, and FTP files. Our team provides fast and accurate verification of both primary and secondary coverage details, including member ID, group ID, coverage period, co-pay, deductible, and co-insurance, using the best possible channels for efficient payer connection. We leverage Robotic Process Automation to improve speed and accuracy while identifying and resolving any missing or invalid data. Our service also includes verifying patient demographic and policy information, such as benefits, deductibles, plan inclusions, and exclusions, along with obtaining pre-certification numbers and approvals. We ensure prompt verification of patients’ coverage, co-pays, co-insurance, deductibles and claims mailing addresses on all primary and secondary payers, keeping your revenue cycle management system updated.
Say goodbye to insurance-related headaches and enjoy a streamlined verification process with Sun Knowledge! For more information, reach out to us today!
